When Is a Tooth Extraction Necessary? Sweet Water Dentistry | Fairhope, Alabama A Gentle Approach to a Tough Decision At Sweet Water Dentistry in Fairhope, Alabama, we believe that your natural...
Dental Care for Aging Parents and Grandparents
Dental Care for Aging Parents and Grandparents As our loved ones age, their dental needs change — and often become more complex. From managing dry mouth and gum disease to adjusting dentures or...
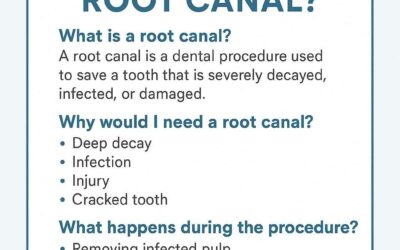
What Is a Root Canal? Understanding the Basics
🦷Series 1: What Is a Root Canal? Understanding the Basics Hearing the words "root canal" can make anyone a little uneasy—but there’s no need to fear! At Sweet Water Dentistry, we believe in helping...
Emergency Dental Care: What to Do in Urgent Situations
Emergency Dental Care: What to Do in Urgent Situations Sweet Water Dentistry, Fairhope, AL Emergencies can happen at any time, and dental issues are no exception. Whether it's a sudden toothache, a...
Are There Alternatives to a Root Canal? Exploring Your Best Options
Are There Alternatives to a Root Canal? Exploring Your Best Options Root canals have long been a go-to treatment for saving severely damaged or infected teeth. However, many patients seek...
How Do I Know If I Need a Root Canal?
How Do I Know If I Need a Root Canal? A root canal is one of the most common dental procedures, yet many people fear it due to misconceptions about pain and complexity. However, modern dentistry has...
What Are the Signs of an Infected Tooth? A Complete Guide to Symptoms and Treatment
What Are the Signs of an Infected Tooth? A Complete Guide to Symptoms and Treatment A tooth infection, also known as a dental abscess, is a painful condition that can lead to serious health...
Best Dentist in Fairhope, AL
Discover the Best Dentist in Fairhope: Sweetwater Dentistry When it comes to your oral health, finding the right dentist is crucial. For families in Fairhope, AL, Sweetwater Dentistry stands out as...
Dentist Near Fairhope, AL
Finding the Best Dentist Near Fairhope for Your Family’s Needs When it comes to your oral health, choosing the right dentist near Fairhope is essential for maintaining a confident smile and...
Porcelain Veneers in Fairhope, AL
Porcelain Veneers in Fairhope, AL The Benefits of Porcelain Veneers: Transform Your Smile with the Best Dentist in Fairhope A confident smile can transform your appearance and how you feel...